Shin Splints – Medial Tibial Stress Syndrome
A common injury in Runners
What is Shin Splints?
It is another very common injury in runners and according to a recent research review shin splints accounts for around 16% of all running-related injuries. It is also referred to as ‘medial tibial stress syndrome’ (MTSS) but both terminologies are used to describe exertional lower leg pain along the inner shin bone (tibial border). It is a diffuse pain, covering an area of 5cm or more rather than a localised pain. The pain in you lower leg can be bone related and non-bone related. It is therefore important that you get assessed by an experienced physiotherapist or a sports doctor to ensure that a more serious diagnosis such as a stress fracture is not suspected. This type of injury would require more acute immobilisation and careful management.
How do you know what causes the pain?
Bone related pain
This is one cause related to the MTSS and it is caused by stress and inflammation to the inside of your shin bone (tibia). Continuous stress can result in periostitis, which is an inflammation and irritation of the membrane surrounding the tibia. This happens at the early stages of MTSS and causes soreness along the inner border of the tibia. Compared to a stress fracture, the pain of periostitis often presents over a larger area whilst a stress fracture is a much more localised pain. However, if there is continuous stress to the bone this could result in bone oedema (swelling) and there is also an increased risk of developing a stress fracture.
When should you suspect a stress fracture?
- If shin pain gets increasingly more painful during the run. However, this can also be the case with severe bone inflammation. Pain from MTSS is usually worse at the beginning of the run and improves, or goes away once the muscles have warmed up during the run.
- If you can localise a focal point of sharp pain along the shin bone (tibia). MTSS usually presents with pain over a larger more diffuse area.
- Stress fractures are usually better in the mornings due to the rest overnight. Whilst MTSS is often worse in the morning due to increased soft tissue tightness.
This is a very simplistic way of identifying stress fracture so if this condition is suspected it is important to get a proper assessment done by a doctor or physio. Sometimes imaging will be required to ensure that you get the right diagnosis.
Muscular related pain
Muscular shin pain is much less common and this condition is called Chronic Exertional Compartment Syndrome (CECS). The pain most often experienced in the front part of the shin. Many runners describe it as a tightening of the shin that gets worse during exercise. The pressure within the muscle increases during exercises and the fascia surrounding the muscle gets squeezed leading to the pain and tightening feeling.
Runners are usually pain-free at rest but they may also experience some neurological symptoms, such as numbness, tingling or weakness in the foot. This is can be due to compromised neurovascular function and medical advice should be sought.
What causes shin splints?
There are several risk factors for developing shin splints. It is mainly seen as an ‘overuse’ injury and beginners are more susceptible but also runners returning to harder training after an injury, rest or illness are at increased risk of developing MTSS.
The most common causes are:
- Sudden increase of running volume and intensity.
- Poor biomechanics; such as overpronation of foot, flat feet, dropped arches and poor hip rotation.
- Low bone density; This is important to bear in mind when it comes to female athletes as some may suffer from secondary amenorrhoea, low energy availability and osteoporosis, known as the female athlete triad . This is a complex condition that is linked to the broader and more comprehensive term, Relative Energy Deficiency in Sports (RED-S). Coaches and athletes should be aware of this condition so it can be picked up early and specialist input may be required. It affects many aspects of physiological function, health and athletic performance as well as increasing the risk of developing stress fractures.
- Tight calf muscles, which can increase loading on the shin.
- Wrong running shoes; for example, poor cushioning, worn-out and poor support.
How can we treat Shin Splints?
- Stop running: unfortunately, with most shin splints you have to take some rest from running. This period varies depending on how severe the inflammation is but usually a 1-2 week break will be needed with no ‘test runs’ every few days! If you get acute pain during your sessions, stop and don’t keep on completing your training in pain as this will eventually prolong recovery and worsen your diagnosis. During this time fitness levels can be maintained through aqua-jogging, cycling (if pain-free), swimming and weight training (no stress on lower leg).
- Icing: I would recommend to ice the painful area (wrap ice around a thin towel to avoid skin injury). Ice for 3x5min (2min break in between), 3 times a day.
- Anti-inflammatories: it is important not to use medication to mask pain as the pain can be helpful in monitoring the healing process. However, for MTSS anti-inflammatories such as Ibuprofen gel or Diclofenac gel can be used to reduce inflammation. This is not recommended if stress fracture is suspected as it may delay bone healing.
- Foot assessment: get a biomechanical foot assessment to ensure you get the right support, correct shoes or the need for orthotic insoles. As mentioned overpronation can be a risk factor for shin splints.
- Correct causes of over-pronation: exercises for ankle and calf stretches and gluteus medius strengthening exercises can help to prevent biomechanical causes of over-pronation.
How can we Prevent Shin Splints?
- Well planned Training program
- It is important to build up the distance and intensity in a gradual and sensible way.
- Find an experienced coach that you can discuss your aims and goals with.
- Good foundation
- Include strength and conditioning, technical work and flexibility.
- Calf strengthening and stretching exercises
- Running drills; works on putting your strength training and running training into the correct biomechanical movements. Most drills focuses on foot placements, stability and control which will improve your running technique and reduce risk of injuries, including shin splints.
- General stretching of lower limb muscles to enhance recovery, prevent stiffness and tightness of muscles and tendons.
- Ankle and Foot Stability
- As mentioned above, poor foot or ankle control can also cause pronation of foot and lead to valgus knee which increases strain on the tibia.
- Poor foot arch control and flat feet also has this effect on valgus and lower leg problems.



1.Pronation of foot – 2.Knee valgus – 3.Correction with insoles
- Footwear assessment: Sometimes a formal assessment is useful to find out if you are flat footed or pronating/supinating. Appropriate running shoe and sometimes orthotics are important to ensure you avoid injuries such as the MTSS.
- Change your shoes regularly if your distance is building up. It is recommended that you change your running shoes after 500-800km, so if you run 30km/week you should change your shoes every 4-6 months.
4. Optimising Bone Density
- Ensure 1.3g calcium and 400mcg Vitamin D per day to protect your bone health.
- Female athletes also need to think about the risk associated with low energy availability (low calorie intake), amenorrhoea and osteoporosis. As mentioned above ‘Female Athlete Triad’
- Iron supplementationshould also be considered in athletes with ferritin below 35 µg/L. As iron deficiency is associated with female athlete triad it is important to optimise iron levels for this group of endurance athletes.
What Exercises can help prevent and manage MTSS?
Ankle Strengthening:
- Flexion and extension
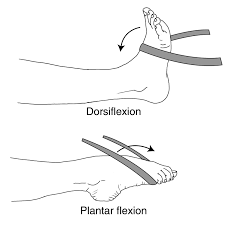
- Eversion and Inversion

Gluteus exercises can prevent valgus and pronation of foot:
- Gluteus strengthening exercises (examples):
Clam exercise

Lunges (with or without weights)

Hip thrusts


Step-ups (with or without weights)

Stretching
- Calf Stretches
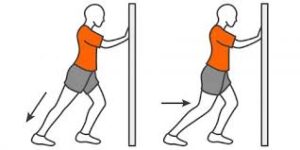

Gastrocemius VS Soleus stretch
Important to stretch both calf muscles
3x30sec on both legs
- Anterior Tibialis stretching
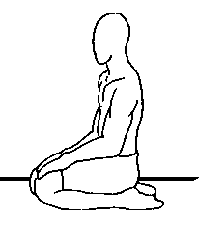
Sit on you shins with your feet plantar flexed.
Hold for 30sec then rest for 30sec. Repeat 3 times.
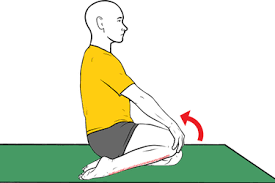
Same as above but to add more stretch you lift one knee up at a time.
Hold for 30sec then rest for 30sec. Repeat 3 times. Alternate the legs.
Sports massage & myofascial release:
-
This may be beneficial after the acute phase. The massage can reduce tension in the calf muscles and the anterior tibias muscle, which may be causing excessive traction forces on the bone.
-
It also increases the blood flow and therefore aiding the healing process.
-
However, it is important to see an experiences sports masseur so that the technique is correct and further irritation to the inflamed periosteum is avoided.
Taping
- Kinesio tape (KT tape) can help in releasing some pain and discomfort. The thought is that it helps to ‘lift’ the superficial tissues’, increase blood supply to the inflamed area which improves healing

- The efficacy of KT on shin splints is still not clear. However, some studies show that runners who used KT tape experiences less pain and improved function compared to runners who only used shoe insoles.
- The tape can be left on up to a week if applied properly but it would be important to choose a tape that provides strong adhesion and support.
When can you return to normal training again?
Well, this is very individual and would strongly depend on the severity of your condition as well as the root cause of the problem.
The aim is to return to running once you are pain-free at rest and at walking. Together with your physio, sports doctor and coach you should reintroduce running cautiously with alternating running and walking to start off with.
Tips for return to training:
- Acute phase:
- Exclude more serious cause such as Stress Fracture
- No running for around 2 weeks to start off with.
- Alternative training methods: aqua-jogging, strength training, swimming, cycling (if pain-free during cycle and after) to maintain fitness level and work on any weaknesses.
- Mobilisation: stretching and flexibility training
- Icing
- Massage
- Taping
- Review potential causes of injury:
- Sudden changes in training program
- Shoes
- Foot/ankle stability
- Supplements Iron, Calcium and Vit D
- Recovery Phase (1-4 weeks)
- Once pain-free at rest and on walking
- Slowly reintroduce low intensity running mixed with walking
- If any pain during running or after running then I advise review with your physio or sports doctor to ensure that return to training is carefully managed and other causes should be re-considered.
- In some cases, running has to be delayed further but you can continue with all alternative training methods that is not causing pain or putting excessive stress on the shin (tibia)
- This phase can vary depending on severity and cause but usually a gradual return to full training should be possible within 4 weeks in most cases if pain-free.
- MTSS usually responds well to rest so if pain comes back or is not fully resolved then further assessment with an experienced sports doctor is recommended.
- Stick to the 10% Rule
- Don’t increase your weekly distance by more than 10% as it is important to give your body time to adjust and this will also keep injuries away!
- Once pain-free at rest and on walking






